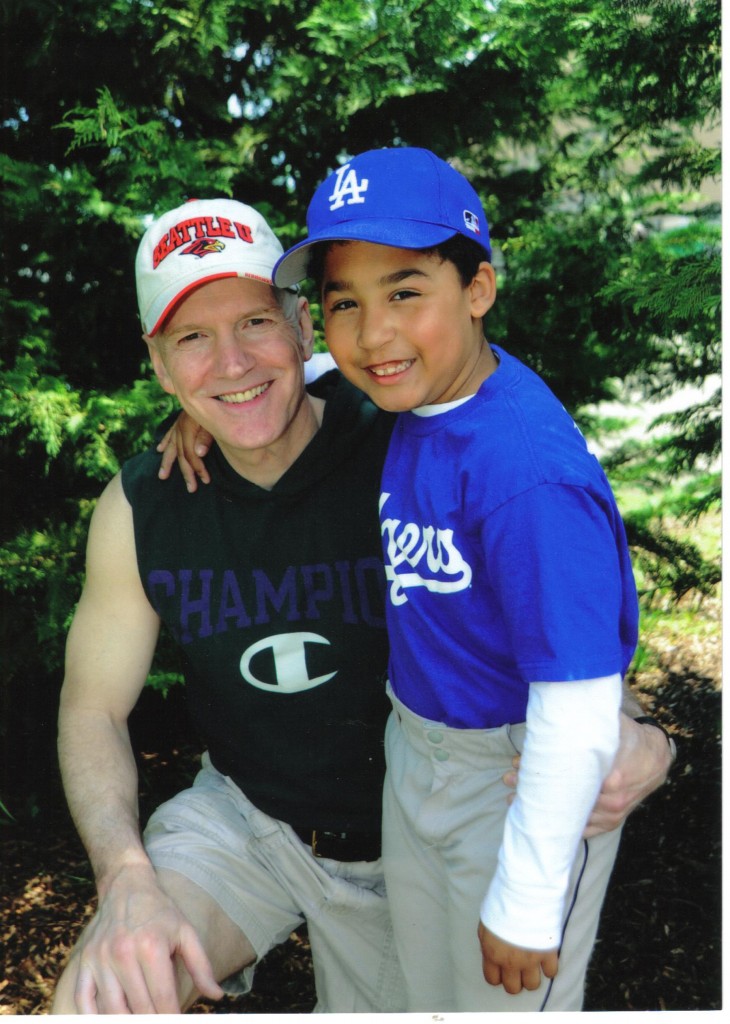
Clay Moyle and son Caleb
This article is for the older broken down readers like me, those of you who might one day find yourself in need of a hip replacement.
A couple of weeks ago I learned of a fellow from Bainbridge Island a few years older than myself who was going to get a hip replacement. Since I already have a couple of artificial hips I reached out to him to try and make him aware of the hip resurfacing option.
Unfortunately, by the time he phoned me back he left a message advising that he’d already had a total hip replacement so there really wasn’t any point in sharing my views on the difference between the two with him.
Modern total hip replacements were first performed in the early 1960s. Hip replacements are considered by many to be the most important operation developed in the 20th century in terms of the relief of human suffering.
Prior to the option of having a hip replacement those unfortunate souls who suffered from arthritis in the joint were doomed to a life of pain and very limited mobility. I had a taste of that before my first replacement when I was in a constant state of pain as a result of the loss of cartilage in that joint.
I read somewhere that the surface of normal human cartilage is supposed to be slipperier than a puck on ice. But, arthritic cartilage may be cracked, or worn through to the bone and doesn’t glide well. An arthritic join may be very stiff and feels like it grinds, catches or worse yet locks, when one attempts any movement.
There’s also a lot of pain associated with that.
Just prior to my first hip replacement in 2005 I had reached the point where anytime I sat down for more than a few minutes and tried to stand up the joint would be locked up. I’d very slowly stand up and straighten that leg out while suffering excruciating pain before I could put some weight on it and begin walking.
As a result, I didn’t feel like doing much of anything, and although I was still going to the gym and working out to stay in some kind of condition it had literally become a real grind.
Approximately 80 percent of patients with arthritic hips will discover it as a result of some pain in the groin or front side of thigh. When they visit an orthopedic surgeon the doctor will typically be able to determine if they have an arthritic hip simply by putting them on their back and lifting they leg bent at the knee and moving it around a bit.
Based on the result of that physical examination they’ll typically order plain X-rays and if they have arthritis it will normally be very evident by the loss of cartilage and corresponding narrowness of the space between the bones in the joint.
At this time, the only long-term solution in terms of relief from an arthritic hip is hip replacement surgery. Hip replacement involves surgically removing the arthritic parts of the joints (cartilage and bone), replacing the “ball and socket” part of the joint with artificial implants and placing a high-performance bearing surface between the metal parts.
Usually, the bearing surface is made from a very durable polyethylene plastic. But other materials including ceramics, plastics or metals are also used.
Patients typically spend three to four days in a hospital after the surgery and are essentially bed-ridden for the better part of three weeks while they recover.
Most patients will use either a walker or crutches to get around during that period of time and will find that they don’t have much energy as their body goes through the healing process.
The patient is typically administered morphine for the first couple of days after the surgery and then switched over to a pain reliever like Vicodin or Percocet for the next few weeks.
There are three types of hip replacement surgery. The first is a total hip replacement where the entire hip joint (ball and socket, as well as the femoral stem) is replaced. That is the more traditional replacement and the only one that the initial surgeon I consulted with even told me about.
The second is a partial hip replacement where only the ball (femoral head) is replaced.
Finally, there is a hip resurfacing procedure where the cup is replaced but the ball is not. Instead, the ball is reshaped and covered with a metal cap and the patient retains their femoral stem. In the case of a hip resurfacing procedure the patient retains 85-90 percent of the femoral head and neck.
I was only two weeks away from a total hip replacement when I learned of the hip surfacing option. I immediately phoned my surgeon to inquire about that option and he told me he had no intention of every doing them.
Early hip resurfacing attempts apparently resulted in a number of fractures of the femoral neck and there were concerns about the long-term success of that method because of the failure of some of the materials that were initially used.
But, I did more investigation and arranged for a consultation with one of only two doctors (Dr. James Pritchett) that were performing hip resurfacing procedures in the area at the time.
Dr. Pritchett assured me that there was every reason to believe the hip resurfacing option would be a much more satisfactory solution for a man my age and convinced me that I would have every chance of being much more physically active afterward if I opted for that type of surgery.
The thought of retaining as much 85-90 percent of the femoral bone so that I’d still have other options further down the road made a lot of sense to me. The fact that hip resurfacing would offer added stability as a result of the larger diameter of the prosthetic implant covering the femoral head and enable a more accurate restoration of leg length and placement angle of the joint was also very appealing.
On the flip side, I learned that the hip resurfacing procedure was a more invasive surgery than a total hip replacement. When a traditional hip replacement is performed they are able to make a smaller incision because they’re going in and cutting and removing a lot of bone so there is more room for them to work.
By comparison, when a surgeon performs a hip resurfacing procedure they have to make a larger incision and they actually dislocate your hip and do some cutting of supporting tissue so they can make enough room to perform the procedure.
Hip resurfacing is a more complicated and slightly longer procedure. When I watched a video of the surgery performed on another party after my first operation I came to understand why I was so dang sore for weeks afterward.
Another concern with the hip resurfacing procedure is the use of metal-on-metal implants as opposed to plastic or ceramic components. Cobalt chromium implants were used for my bionic parts.
All patients with metal-on-metal hip implants have elevated levels of cobalt in their hair, blood, urine and vital organs. As the cobalt is generated it has to be absorbed by the lymphatics and synovial tissues. It is then circulated and excreted through the urine.
As the recipient of metal-on-metal implants move their legs the surfaces of those components rub against each other. The friction and wear between the components causes debris, regardless of how microscopic. Obviously, in the case of the use of cobalt chromium implants the debris is cobalt.
It’s possible that the debris can cause a condition known as metallosis.
Metallosis is a rare condition caused by the buildup of metallic debris in the soft tissue of the body – in this case the soft tissue surrounding the hip joint.
It’s more typically seen in hip resurfacing patients than in total hip replacement patients because most hip resurfacing implants are used in younger, more active individuals who tend to put a higher level of wear and tear on the implants than older folks.
Additionally, hip resurfacing implants tend to have a larger femoral ball which tends to cause more abrasive wear within the joint and thereby produces more metallic debris.
It’s possible that metal debris can lead to oxygen starvation of the surrounding tissue and ultimate death of that tissue. The full impact of metallosis isn’t known but it’s been linked to various replacement complications.
Obviously, the idea of the release of metal ions inside my body concerns me. My surgeon believes that the incidence of metallosis from metal-on-metal hip resurfacing may not be as common as feared. I hope to heck he’s right.
As for the longevity of the implants, my surgeon advised that there’s no long-term track record yet for the materials that he used for me but he told me there’s no reason they shouldn’t last longer than the surrounding bone.
Patients who receive total hip replacements are typically told to stick with low-impact activities afterward including swimming, water aerobics, cross-country skiing, cycling and golf.
In contrast, many surgeons who perform hip resurfacing procedures on their patients place no such restrictions on their patients and give them the green light to resume such high-impact activities as basketball, hockey, racquetball, etc. after a six-month waiting period.
Six months after the hip resurfacing procedure is considered the window within which femoral neck fractures will most commonly occur.
So, seven years ago and shortly after my second hip replacement operation, I specifically asked my surgeon about the possibility of returning to playing full court basketball. He told me there were no restrictions and to proceed. The only thing he cautioned me about was taking offensive charges as he felt it would be wise to avoid crashing to the floor as much as possible.
Now, obviously I realize that by playing basketball and remaining as active as I am in other ways that I am increasing the risk of wearing the implants out sooner. I’m also somewhat concerned about this issue of the release of metal ions in my body but overall I’m of the opinion that there are obvious disadvantages with any form of hip replacement surgery and I’m comfortable that I made the right decision for myself.
It still amazes me to think of the stage I’d reached in terms of the arthritic condition of my hips and limited mobility eight years ago and the fact that I’m now running up and down the court and competing with men as much as 25-35 years younger every weekend.
However, I will add that I feel great for three straight games of basketball. But, if I push it and play four or five in a row I tend to suffer from inflammation in my hips, and especially the right one. And I walk very stiffly as a result for the rest of the day. So, I question my sanity when I push it to that point.
Still, I’m thankful that I live in a time where hip replacements are an option and I won’t have to spend the balance of my life in pain and inactive.
Hopefully, they’ll figure out a way to regenerate cartilage in the future so the quality of life for future generations will be even further improved and metal, plastic or ceramic implants won’t be necessary at all.
In the meantime, I encourage anyone facing hip replacement surgery to do their homework so they can make an educated decision as to the best course of action for themselves.